Judgment and Classification of Hypoxia
Why is there hypoxia?
Oxygen is the main substance that sustains life. When tissues do not receive enough oxygen or have difficulty in using oxygen, causing abnormal changes in the body’s metabolic functions, this situation is called hypoxia.
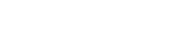
Basis for judging hypoxia
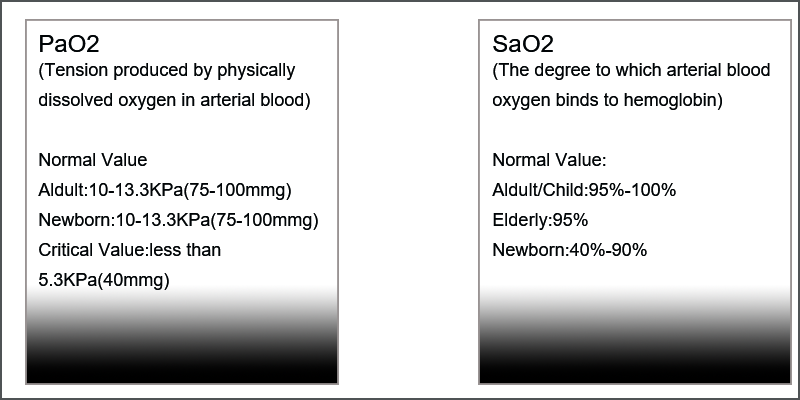
Hypoxia degree and symptoms
Classification of hypoxia
| Classification of hypoxia | arterial partial pressure of oxygen | arterial oxygen saturation | Arteriovenous oxygen difference | Common causes |
| hypotonic hypoxia | ↓ | ↓ | ↓ and N |
Low oxygen concentration in the inhaled gas, dysfunction of external exhalation, venous shunt into arteries, etc. Commonly seen in chronic obstructive pulmonary disease and congenital heart disease such as tetralogy of Fallot. |
| blood hypoxia | N | N | ↓ |
Reduced amount or altered properties of hemoglobin, such as anemia, carbon monoxide poisoning, and methemoglobinemia. |
circulatory hypoxia |
N | N | ↑ | It is caused by reduced tissue blood flow and reducedtissue oxygen supply, which is common in heart failure,
shock, etc. |
organizational hypoxia |
N | N | ↑ or ↓ |
Caused by abnormal utilization of oxygen by tissue cells, such as cyanide poisoning. |
Oxygen inhalation therapy and its purpose
Under normal conditions, healthy people breathe air naturally and use the oxygen in it to maintain metabolic needs. When illness or certain abnormal conditions lead to hypoxia in the body, certain equipment must be used to supply oxygen to the patient, increase arterial oxygen partial pressure (PaO2) and oxygen saturation (SaO2), improve hypoxia, promote metabolism, and maintain life. Activity.
Benefits of oxygen inhalation
- Relieve angina pectoris and prevent myocardial infarction
- Prevent sudden death from coronary heart disease
- Good treatment for asthma
- Effectively treats emphysema, pulmonary heart disease, and chronic bronchitis
- Oxygen inhalation has an auxiliary therapeutic effect on diabetes: current research shows that diabetes is related to the body’s lack of oxygen. Diabetic patients have significantly lower capillary pressure, and tissue cells cannot fully obtain oxygen, leading to impairment of cell function and glucose metabolism. Therefore, the implementation of oxygen therapy for diabetic patients has attracted the attention of the medical community.
- Oxygen inhalation can play a health care role in healthy people: air pollution, common use of air conditioning, regular oxygen inhalation can clean the respiratory system, improve internal organ function, enhance the body’s comprehensive immunity, and prevent various diseases.
What are the classifications of oxygen therapy?
- High concentration oxygen supply (5-8L/min):It is used for acute respiratory failure such as respiratory and cardiac arrest, acute respiratory distress syndrome, acute poisoning (such as carbon monoxide poisoning or gas poisoning) respiratory depression, etc., where high concentration or pure oxygen must be used every second for rescue, but it is not suitable for long-term use. to prevent oxygen poisoning or other complications.
- Medium concentration oxygen supply (3-4L/min):It is suitable for patients with anemia, cardiac insufficiency, shock, etc. who do not have strict restrictions on the concentration of inhaled oxygen.
- Low concentration oxygen supply (1-2L/min):Generally used for chronic bronchitis, emphysema, pulmonary heart disease, etc., also known as chronic obstructive pulmonary disease. Too high blood oxygen partial pressure can weaken the reflex stimulation of the carotid sinus to the respiratory center, thereby reducing ventilation and aggravating carbon dioxide retention. possible. Therefore, oxygen should be used with caution, and low-concentration continuous oxygen inhalation is generally used.
Oxygen concentration and oxygen flow
Oxygen concentration: The proportion of oxygen contained in the air. The oxygen concentration in normal atmospheric air is 20.93%
- Low concentration oxygen <35%
- Medium concentration oxygen 35%-60%
- High concentration oxygen >60%
Oxygen flow: refers to the adjusted oxygen flow for patients, unit L/min.
Oxygen concentration oxygen flow conversion
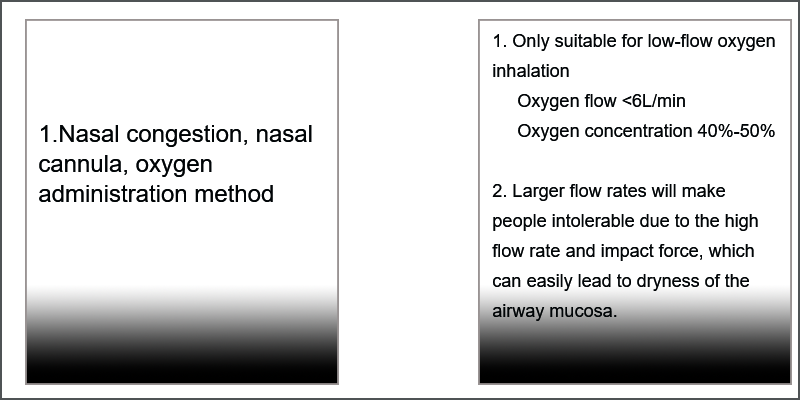
- Nasal cannula, nasal congestion: Oxygen concentration (%) = 21+4X oxygen flow (L/min)
- Mask oxygen supply (open and closed): flow rate must be greater than 6 L/min
- Simple respirator: oxygen flow rate 6 L/min, inhaled oxygen concentration approximately 46%-60%
- Ventilator: Oxygen concentration = 80X oxygen flow (L/min) / ventilation volume + 20
Classification of oxygen therapy-According to oxygen supply method
Things to note when using oxygen
- Safe use of oxygen:Effectively implement the “four preventions”: earthquake prevention, fire prevention, heat prevention, and oil prevention. At least 5 meters away from the stove and 1 meter away from the heater. The oxygen cannot be used up. When the pointer on the pressure gauge is 5kg/cm2, it cannot be used again.
- Strictly abide by the oxygen operating procedures:When using oxygen, you should use it first. When stopping, pull out the catheter first and then turn off the oxygen. When changing the flow rate midway, you should separate the oxygen and nasal catheter first, adjust the flow rate before connecting.
- Observe the effect of oxygen use: cyanosis is alleviated, heart rate is slower than before, dyspnea is relieved, mental state is improved, and trends in various indicators of blood gas analysis, etc.
- Change nasal cannula and humidification solution every day (1/3-1/2 full of distilled or sterilized water)
- Ensure emergency use: unused or empty oxygen cylinders should be hung with “full” or “empty” signs respectively.
Main precautions for oxygen inhalation
- Closely observe the effect of oxygen therapy: If symptoms such as dyspnea are reduced or relieved, and the heartbeat is normal or close to normal, it indicates that oxygen therapy is effective. Otherwise, the cause should be found and dealt with in time.
- High-concentration oxygen supply should not be provided for too long. It is generally believed that if the oxygen concentration is >60% and continues for more than 24 hours, oxygen poisoning may occur.
- For patients with acute exacerbation of chronic obstructive pulmonary disease, controlled (i.e. low-concentration continuous) oxygen inhalation should generally be given.
- Pay attention to heating and humidification:Maintaining a temperature of 37°C and a humidity of 95% to 100% in the respiratory tract is a necessary condition for the normal clearing function of the mucociliary system.
- Prevent contamination and duct blockage:Things should be changed and cleaned and disinfected regularly to prevent cross-infection. Catheters and nasal obstructions should be checked at any time to see if they are blocked by secretions and replaced in time to ensure effective and safe oxygen therapy.
Standards for prevention and treatment of common complications of oxygen inhalation
Complication 1: Dry respiratory secretions
Prevention and treatment: The oxygen coming out of the oxygen supply device is dry. After inhalation, it can dry the respiratory mucosa and make the secretions dry and difficult to discharge. Distilled water should be added to the humidification bottle, and sterilized water should be added to humidify oxygen.
Complication 2: Respiratory depression
Prevention and treatment: During hypoxemia, the decrease in PaO2 can stimulate peripheral chemoreceptors, reflexively excite the respiratory center, and increase lung ventilation. If the patient relies on this reflex excitation to maintain breathing for a long time (such as patients with pulmonary heart disease and type II respiratory failure), inhaling high concentrations of oxygen can eliminate this reflex mechanism, inhibit spontaneous breathing, and even cause Breathing stops. Therefore, it is necessary to provide low-flow, low-concentration controlled oxygen and monitor changes in PaO2 to maintain the patient’s PaO2 at 60mmHg.
Complication 3: Absorptive atelectasis
Prevention and treatment: After a patient inhales high concentrations of oxygen, a large amount of nitrogen in the alveoli is replaced. Once the bronchus is blocked, the oxygen in the alveoli can be rapidly absorbed by the circulating blood flow, causing the alveoli to collapse and cause atelectasis. Therefore, preventing respiratory obstruction is key. Measures include encouraging patients to take deep breaths and coughs, strengthening sputum discharge, changing body positions frequently, and reducing oxygen concentration (<60%). Patients on ventilators can be prevented by adding positive end-expiratory pressure (PEEP).
Complication 4: Retrolental fibrous tissue hyperplasia
Prevention and treatment: After using high-concentration oxygen, excessive arterial oxygen partial pressure (PaO2 reaches more than 140mmHg) is the main risk factor for causing retrolental fibrous tissue hyperplasia in newborns (especially premature infants). Therefore, the oxygen concentration of newborns should be strictly controlled below 40%, and the oxygen inhalation time should be controlled.
Complication 5: Oxygen poisoning
Clinical manifestations:
- Symptoms of pulmonary oxygen poisoning: retrosternal pain, dry cough and progressive dyspnea, reduced vital capacity
- Symptoms of cerebral oxygen poisoning: visual and hearing impairment, nausea, convulsions, syncope and other neurological symptoms. In severe cases, coma and death may occur.
- Manifestations of ocular oxygen poisoning: retinal atrophy. If premature infants take oxygen for too long in the incubator, the retina will have extensive blood vessel occlusion, fibroblast infiltration, and retrolental fiber proliferation, which can lead to blindness.
Post time: Nov-21-2024