“Within critical care medicine, silent hypoxemia persists as an underrecognized clinical phenomenon with grave implications. Characterized by oxygen desaturation without proportional dyspnea (termed ‘silent hypoxia’), this paradoxical manifestation serves as a critical indicator of impending respiratory failure. Mounting evidence confirms its role as a stealthy pathophysiological mechanism, with delayed diagnosis contributing to preventable mortality across pneumonia, COVID-19, and chronic pulmonary conditions. The New England Journal of Medicine recently highlighted this ‘clinician’s paradox’ – where normal respiratory effort masks catastrophic oxygen deprivation, demanding renewed clinical vigilance and monitoring protocol reforms.”
What is hypoxemia?
“Hypoxemia, defined as a pathological deficiency of oxygen saturation in arterial blood (PaO2 < 80 mmHg at sea level in adults), arises when partial pressure falls below age-adjusted normative thresholds (AARC Clinical Practice Guideline 2021). High-risk cohorts demonstrate distinct pathophysiological profiles:
- Ventilation/Perfusion mismatch: Severe pneumonia patients with alveolar infiltrates impairing diffusion capacity
- Cardiogenic mechanisms: Left/right heart failure cohorts exhibiting pressure-induced pulmonary edema (PCWP >18 mmHg)
- Neuromuscular compromise: Pediatric populations with underdeveloped intercostal musculature and adults with diaphragmatic dysfunction
- Chronic exposure: Tobacco users manifesting structural lung changes (emphysema, COPD-GOLD stage ≥2)
- Iatrogenic triggers: Postoperative patients experiencing opioid-induced respiratory depression (RR <12/min) and atelectasis
Notably, 38% of thoracic surgery patients develop hypoxemia within 24h post-extubation (ASA Closed Claims Data 2022), underscoring the necessity of continuous pulse oximetry monitoring in these populations.”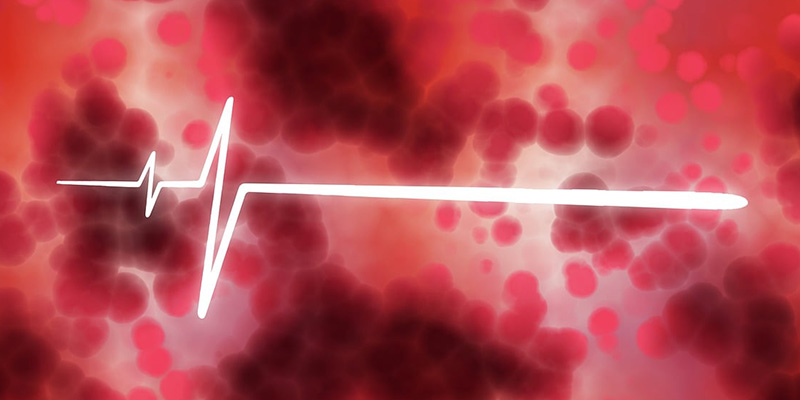
What are the dangers of hypoxemia?
According to clinical statistics, the mortality rate of patients with severe hypoxemia can reach 27%, and in more serious cases, the mortality rate can even reach more than 50%. If timely intervention is not made in the early stages of the disease, serious consequences are likely to occur.
- Impact on the brain: When blood oxygen levels drop (hypoxemia), the brain becomes deprived of oxygen. This can trigger immediate symptoms like persistent headaches, sudden dizziness, and memory lapses. If left untreated, prolonged oxygen starvation may damage brain cells, potentially leading to strokes caused by blocked blood flow (cerebral infarction) or ruptured blood vessels (cerebral hemorrhage). Early recognition of these warning signs is critical to prevent permanent neurological damage.
- Impact on the heart: When the heart doesn’t get enough oxygen, it struggles to pump effectively. This strain can trigger warning signs like rapid or irregular heartbeat, chest tightness (angina), and unusual fatigue. Over time, untreated oxygen deprivation may weaken the heart muscle, potentially leading to life-threatening complications such as heart failure, where the heart can’t keep up with the body’s needs.
- Impact on the lungs: Low oxygen levels force the lungs to work harder just to keep up. Over time, this strain can damage airways and lung tissue, increasing the risk of developing breathing disorders like COPD (chronic obstructive pulmonary disease). In severe cases, prolonged oxygen deprivation may even weaken the right side of the heart as it struggles to pump blood through stiffened lungs, a condition known as cor pulmonale.
- Whole-body effects: Chronic oxygen shortage strains every organ like a car running on low fuel. Kidneys and liver gradually become less efficient at filtering toxins, while the immune system weakens, making common infections harder to fight. Over time, this silent oxygen debt increases risks of organ damage and leaves the body vulnerable to cascading health problems – from frequent illnesses to lasting organ scarring. This makes early oxygen level monitoring crucial for preventing multi-organ complications.
How to determine if you have hypoxemia?
Blood oxygen levels are a key measure for detecting oxygen deficiency. In healthy individuals, normal readings range from 95% to 100%. Levels between 90-94% indicate mild oxygen shortage, which may not show obvious symptoms. A drop to 80-89% signals moderate oxygen deprivation, often causing labored breathing or confusion. Readings below 80% represent a severe emergency, where vital organs risk damage due to extreme oxygen starvation and require immediate medical attention.
How to maintain normal blood oxygen saturation?
- Open windows for ventilation
Refresh your indoor air by opening windows daily to circulate fresh oxygen. For better results, periodically visit parks or nature-rich areas outside urban zones to take deep, clean breaths that help recharge your body’s oxygen levels.
- Aerobics
Regular aerobic activities like brisk walking, swimming, or cycling can boost blood flow and oxygen circulation. Choose low-intensity options like water aerobics or slow jogging if you’re new to exercise – these gentle workouts safely improve oxygen delivery while building stamina over time.
- Home oxygen therapy
For individuals with chronic breathing conditions who struggle with low oxygen levels, using a home oxygen device can help maintain proper oxygenation. Doctors often recommend starting with portable oxygen concentrators during sleep or daily activities – when used as directed, this therapy can improve energy levels, reduce breathlessness, and support better sleep quality.
Post time: Apr-25-2025