Oxygen is one of the elements that sustain life
Mitochondria are the most important place for biological oxidation in the body. If the tissue is hypoxic, the oxidative phosphorylation process of mitochondria cannot proceed normally. As a result, the conversion of ADP to ATP is impaired and insufficient energy is provided to maintain the normal progress of various physiological functions.
Tissue oxygen supply
Arterial blood oxygen contentCaO2=1.39*Hb*SaO2+0.003*PaO2(mmHg)
Oxygen transport capacityDO2=CO*CaO2
The time limit for normal people to tolerate respiratory arrest
While breathing air:3.5min
When breathing 40% oxygen:5.0min
When breathing 100% oxygen:11min
Lung gas exchange
Oxygen partial pressure in air(PiO2):21.2kpa(159mmHg)
Oxygen partial pressure in lung cells(PaO2):13.0kpa(97.5mmHg)
Mixed venous partial pressure of oxygen(PvO2):5.3kpa(39.75mmHg)
Equilibrated pulse oxygen pressure(PaO2):12.7kpa(95.25mmHg)
Causes of hypoxemia or lack of oxygen
- Alveolar hypoventilation(A)
- Ventilation/perfusion(VA/Qc)Disproportionality(a)
- Decreased dispersion(A-a)
- Increased blood flow from right to left shunt(Qs/Qt Increased)
- Atmospheric hypoxia(I)
- Congestive hypoxia
- Anemic hypoxia
- Tissue toxic hypoxia
Physiological limits
It is generally believed that PaO2 is 4.8KPa(36mmHg) is the human body’s survival limit
The dangers of hypoxia
- Brain: Irreversible damage will occur if oxygen supply is stopped for 4-5 minutes.
- Heart: The heart consumes more oxygen than the brain and is the most sensitive
- Central nervous system:Sensitive, poorly tolerated
- Breathe:Pulmonary edema, bronchospasm, cor pulmonale
- Liver, kidney, other:Acid replacement, hyperkalemia, increased blood volume
Signs and symptoms of acute hypoxia
- Respiratory system:Difficulty breathing, pulmonary edema
- Cardiovascular:Palpitations, arrhythmia, angina, vasodilation, shock
- Central nervous system:Euphoria, headache, tiredness, impaired judgment, imprecise behavior, sluggishness, restlessness, retinal hemorrhage, convulsions, coma.
- Muscle nerves:Weakness, tremor, hyperreflexia, ataxia
- Metabolism:Water and sodium retention, acidosis
Degree of hypoxemia
Mild:No cyanosis PaO2>6.67KPa(50mmHg); SaO2<90%
Moderate:Cyanotic PaO2 4-6.67KPa(30-50mmHg); SaO2 60-80%
Severe:Marked cyanosis PaO2<4KPa(30mmHg); SaO2<60%
PvO2 Mixed venous oxygen partial pressure
PvO2 can represent the average PO2 of each tissue and serve as an indicator of tissue hypoxia.
Normal value of PVO2: 39±3.4mmHg.
<35mmHg tissue hypoxia.
To measure PVO2, blood must be taken from the pulmonary artery or right atrium.
Indications for oxygen therapy
Termo Ishihara propose PaO2=8Kp(60mmHg)
PaO2<8Kp,Between 6.67-7.32Kp(50-55mmHg) Indications for long-term oxygen therapy.
PaO2=7.3Kpa(55mmHg) Oxygen therapy is necessary
Acute Oxygen Therapy Guidelines
Acceptable indications:
- Acute hypoxemia(PaO2<60mmHg;SaO<90%)
- Heartbeat and breathing stop
- Hypotension(Systolic blood pressure<90mmHg)
- Low cardiac output and metabolic acidosis(HCO3<18mmol/L)
- Respiratory distress(R>24/min)
- CO Poisoning
Respiratory failure and oxygen therapy
Acute respiratory failure:uncontrolled oxygen inhalation
ARDS:Use peep, be careful about oxygen poisoning
CO poisoning: hyperbaric oxygen
Chronic respiratory failure: controlled oxygen therapy
Three major principles of controlled oxygen therapy:
- In the early stage of oxygen inhalation (first week), oxygen inhalation concentration<35%
- In the early stage of oxygen therapy, continuous inhalation for 24 hours
- Treatment duration: >3-4 weeks→Intermittent oxygen inhalation (12-18h/d) * half a year
→Home oxygen therapy
Change patterns of PaO2 and PaCO2 during oxygen therapy
The range of increase in PaCO2 in the first 1 to 3 days of oxygen therapy is a weak positive correlation of PaO2 change value * 0.3-0.7.
PaCO2 under CO2 anesthesia is around 9.3KPa (70mmHg).
Increase PaO2 to 7.33KPa (55mmHg) within 2-3 hours of oxygen inhalation.
Mid-term (7-21 days); PaCO2 decreases rapidly, and PaO2↑ shows a strong negative correlation.
In the later period (days 22-28), PaO2↑ is not significant, and PaCO2 further decreases.
Evaluation of Oxygen Therapy Effects
PaO2-PaCO2:5.3-8KPa(40-60mmHg)
The effect is remarkable:Difference>2.67KPa(20mmHg)
Satisfactory curative effect:Difference is 2-2.26KPa(15-20mmHg)
Poor efficacy:Difference<2KPa(16mmHg)
Monitoring and management of oxygen therapy
- Observe blood gas, consciousness, energy, cyanosis, respiration, heart rate, blood pressure and cough.
- Oxygen must be humidified and warmed.
- Check catheters and nasal obstructions before inhaling oxygen.
- After two oxygen inhalations, the oxygen inhalation tools should be scrubbed and disinfected.
- Check the oxygen flow meter regularly, disinfect the humidification bottle and change the water every day. The liquid level is about 10cm.
- It is best to have a humidification bottle and keep the water temperature at 70-80 degrees.
Advantages and Disadvantages
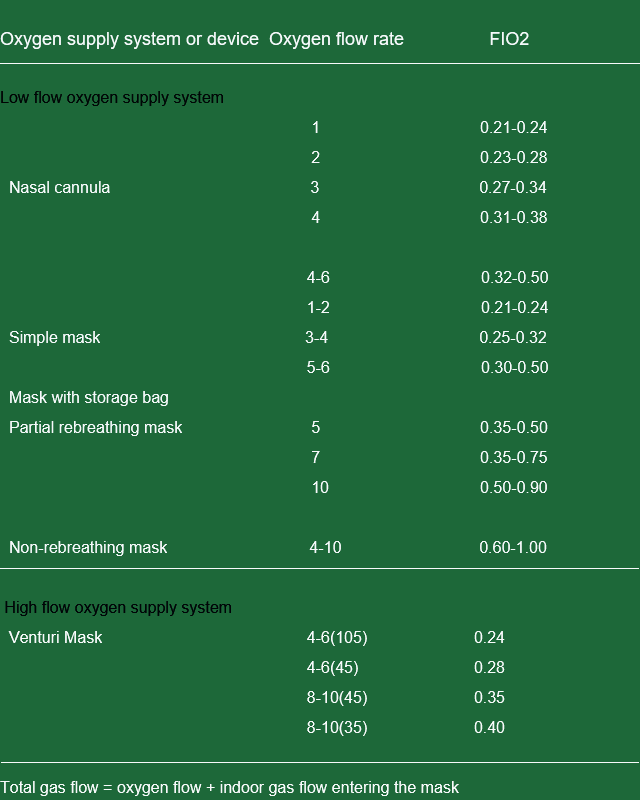
Nasal cannula and nasal congestion
- Advantages: simple, convenient; does not affect patients, coughing, eating.
- Disadvantages: The concentration is not constant, easily affected by breathing; mucous membrane irritation.
Mask
- Advantages: The concentration is relatively fixed and there is little stimulation.
- Disadvantages: It affects expectoration and eating to a certain extent.
Indications for oxygen withdrawal
- Feeling conscious and feeling better
- Cyanosis disappears
- PaO2>8KPa (60mmHg), PaO2 does not decrease 3 days after oxygen withdrawal
- Paco2<6.67kPa (50mmHg)
- Breathing is smoother
- HR slows down, arrhythmia improves, and BP becomes normal. Before withdrawing oxygen, oxygen inhalation must be discontinued (12-18 hours/day) for 7-8 days to observe changes in blood gases.
Indications for long-term oxygen therapy
- PaO2< 7.32KPa (55mmHg)/PvO2< 4.66KPa (55mmHg), the condition is stable, and the blood gas, weight, and FEV1 have not changed much within three weeks.
- Chronic bronchitis and emphysema with FEV2 less than 1.2 liters
- Nocturnal hypoxemia or sleep apnea syndrome
- People with exercise-induced hypoxemia or COPD in remission who want to travel short distances
Long-term oxygen therapy involves continuous oxygen inhalation for six months to three years
Side effects and prevention of oxygen therapy
- Oxygen poisoning: The maximum safe concentration of oxygen inhalation is 40%. Oxygen poisoning may occur after exceeding 50% for 48 hours.Prevention: Avoid high-concentration oxygen inhalation for long periods of time.
- Atelectasis: Prevention: Control oxygen concentration, encourage turning over more often, change body positions, and promote sputum excretion.
- Dry respiratory secretions: Prevention: Strengthen the humidification of the inhaled gas and do aerosol inhalation regularly.
- Posterior lens fibrous tissue hyperplasia: only seen in newborns, especially premature infants. Prevention: Keep the oxygen concentration below 40% and control PaO2 at 13.3-16.3KPa.
- Respiratory depression: seen in patients with hypoxemia and CO2 retention after inhaling high concentrations of oxygen. Prevention: Continuous oxygenation at low flow.
Oxygen Intoxication
Concept: The toxic effect on tissue cells caused by inhaling oxygen at 0.5 atmospheric pressure is called oxygen poisoning.
The occurrence of oxygen toxicity depends on the partial pressure of oxygen rather than the oxygen concentration
Type of Oxygen Intoxication
Pulmonary oxygen poisoning
Reason: Inhale oxygen at about one atmosphere of pressure for 8 hours
Clinical manifestations: retrosternal pain, cough, dyspnea, reduced vital capacity, and decreased PaO2. The lungs show inflammatory lesions, with inflammatory cell infiltration, congestion, edema and atelectasis.
Prevention and treatment: control the concentration and time of oxygen inhalation
Cerebral oxygen poisoning
Reason: Inhaling oxygen above 2-3 atmospheres
Clinical manifestations: visual and auditory impairment, nausea, convulsions, fainting and other neurological symptoms. In severe cases, coma and death may occur.
Post time: Dec-12-2024